Pain management after surgery
We want your stay at Asante to be as comfortable as possible. Though you should expect to have some pain after surgery, your care team will make every effort to safely minimize it. We believe that pain management is an important part of recovery, as well-controlled pain can help you get moving after surgery which can speed healing and lead to fewer complications.
We provide the following information to help you understand your options for pain management, to explain how you can help your care team manage your pain and to help you take an active role in making choices about your pain management.
What kinds of pain will I feel after surgery?
You may be surprised where you feel discomfort. Sometimes you will have discomfort at other sites besides the surgical site. You may or may not experience the following:
Muscle pain. You may feel pain in your neck, shoulders or back from lying on the operating table.
Throat pain. Your throat may feel sore or scratchy; this is from the breathing tube the anesthesia provider inserts after you are asleep.
Pain with movement or activity. Sitting up, walking and coughing — all are important activities after surgery, but they may cause increased pain at or around the surgical site.
What can I do to keep my pain under control?
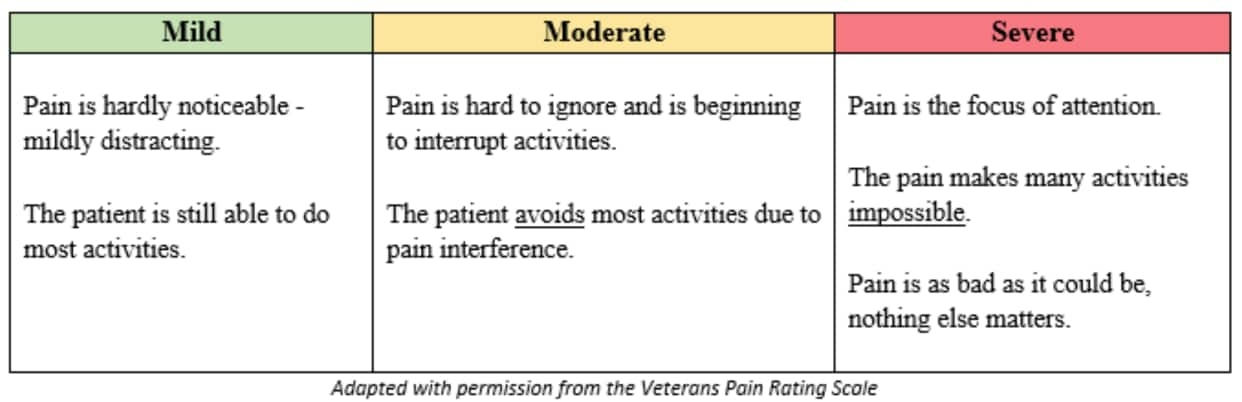
Pain scale
Keep your care team informed of how you’re feeling, especially if pain is limiting your ability to move around. It is unrealistic to expect complete relief from pain following surgery; your goal should be a pain level that you can tolerate but which allows you to get some rest and participate in your postop care, including walking, sitting in a chair, coughing and deep breathing. Your nurses will assess your pain in terms of whether you are able to do these activities, to ensure we are providing the support you need to get on the road to recovery.
Chronic pain. If you have chronic pain before surgery, after surgery you will have surgical pain as well. It is important to tell your care team what medications you take at home and the doses; also tell them your activity level at home and how much discomfort you normally tolerate from chronic pain. If you live at a moderate pain level at home, it may not be possible to safely get your chronic pain to a lower level while in the hospital. If you take narcotics (also called opioids) at home, your body may be less sensitive to pain medication; this is called “tolerance.” It is important to recognize that a person may become tolerant of the pain-relieving effects of opioids, but is still at risk for the side effects. Your care team will work closely with you to keep you safe and as comfortable as possible.
What will be used to treat my pain?
Several methods are used to increase patient comfort and decrease pain after surgery. These include medication, as well as non-medicinal treatments.
Medication. A surgeon takes many considerations into account when ordering pain medication following surgery, including allergies, side effects and appropriate dosage. Your dosing levels will be influenced by your medical condition and diagnosis, as well as your size, age, medical history and whether or not you take pain medication outside the hospital. Your surgeon is responsible for determining which medications you can receive and how often you can take them.
Medications such as Tylenol (acetaminophen) and non-steroidal anti-inflammatory drugs (NSAIDs such as ibuprofen, Advil, Motrin) are helpful in managing pain after surgery and may be ordered by your surgeon.
In addition, narcotics may be ordered and can be given in several different ways. The most common are orally in pill form, intravenously by injection into an IV line, intramuscularly by injection into a muscle, transdermally absorbed through the skin using a patch, or via a patient-controlled analgesia pump. More severe surgical pain may be treated with an epidural or a nerve block, which are medications used to numb a certain area of the body.
- Intravenous patient-controlled analgesia pump. Known as a PCA, this is a computerized pump that safely allows you to push a button to deliver a small amount of pain medication into your IV line. The pump will allow only so much medication — no matter how often you push the button — so there is little worry that you will give yourself too much. One way you can get too much medicine from the pump is if a family member pushes the button for you. Do not allow anyone to push the button for you. This is a major safety feature of the pump; you need to be awake enough to know that you need more medication.
- Epidural analgesia. For pain management in certain types of surgical patients, the anesthesia provider places an epidural catheter that delivers a continuous amount of medication to help desensitize the surgical site. Depending on the type of surgery, the epidural site can vary from the lower back to the middle of the back. While the epidural is in place, you will be monitored closely. The nurse will work with the anesthesia provider to meet your pain goal and keep you comfortable.
During the first 24 hours, your pain level will be monitored frequently, with your oxygen level and breathing monitored continuously. Staff will regularly take your blood pressure, pulse and temperature and will ask about your ability to move your legs and what sensations you are experiencing. All of this is to ensure that the epidural is working correctly to maintain your pain goal while still allowing you to get out of bed and walk. You may need oxygen while the epidural is in place.
- Nerve block. A nerve block controls pain to a small area of the body and is frequently used for orthopedic surgery. One advantage is that a smaller amount of medication can be used, so there are often fewer side effects. A pain pump may be utilized to deliver this medication.

nerve block pain pump
- Non-medicinal treatments. Complementary and alternative modalities can also be used to decrease your pain — and they can supplement the medication you may be receiving. These methods include repositioning with pillows, as well as relaxation such as listening to soothing music and distraction techniques such as watching TV, reading or music therapy. Heat or cold therapy may also be ordered by your surgeon depending on the surgical procedure. Appropriate instructions will be provided for you at discharge if these therapies are ordered.
What are the risks of pain medications?
Side effects. When taking a new medication, anyone can experience side effects that range from mild to life-threatening. Some common, less severe side effects of narcotic pain medications include itching, mild nausea, constipation and drowsiness. The surgeon will frequently order medications to treat these problems, if they occur. More severe side effects can result from getting too much medication; these include the inability to stay awake and decreased breathing.
The nurses will closely monitor you to ensure that the more serious side effects do not occur. We always attempt to balance pain relief with the side effects of the narcotic medication. We will work with you to manage your pain appropriately and safely.
To keep you safe while receiving pain medications in the hospital, you may require extra monitoring, such as an oxygen monitor or a respiratory rate monitor. These monitors alert the nurse if your oxygen level or respiratory rate drops too low.
After receiving pain medication, you may feel unsteady on your feet and need assistance walking or doing routine tasks. To ensure your safety, it’s important to follow the guidelines the nurse, surgeon or physical therapist sets regarding staff assistance when you are out of bed.
What should I know before I am discharged?
The surgeon may prescribe pain medication for you to take at home. If you have any concerns or questions, be sure to ask the nurse. For your safety, it is important to know what medication you are taking, how much to take and when you should take it. Most pain medication prescriptions cannot be called in to a pharmacy. If you are prescribed pain medication for home use, you will be given a written prescription that must be taken in person to an outside pharmacy. If you are traveling from out of state, note that your prescriptions must be filled at a pharmacy in Oregon.
How should I manage my pain at home?
Remember to take your pain medication before activity and when needed, but do not take more than has been prescribed. You should not drive or operate machinery when you are taking narcotics. Check the label of your prescription for any other warnings. Be sure to get enough rest. Use pillows to support yourself when you sleep and when you do your coughing and deep breathing. Try using the alternative methods of pain management mentioned earlier. If your pain is not well controlled, call the surgeon’s office during the day. Some pain medications contain Tylenol, if yours does (check with the surgeon, nurse or pharmacist), extra doses of Tylenol should not be taken. Narcotic pain medications should be used only for as long as necessary.
Here are the most important points to remember about pain management:
- You will not be pain-free after surgery; the nurses will work with you to keep you safe, manage any side effects and keep your pain under control.
- Communicate with the nurses about your pain, and ask any questions you may have.
- Know your pain medication and how to safely take it at home before you leave the hospital.
- Use alternative pain management techniques that minimize the use of narcotic medications.